Rapidly decreasing Prolactin result
| HOSP # | WARD | Endocrinology Clinic | |
| CONSULTANT | John Stanfliet | DOB/AGE | 36 y Female |
Abnormal Result
A low prolactin result was obtained in a patient in whom a macroadenoma was suspected:
Prolactin: 1.3 mIU/L
Presenting Complaint
The patient presented with headache and decreased visual acuity (more specifically peripherally).
History
There were bilateral galactorrhoea, amenorrhoea, and as noted above, headache and visual disturbances.
The patient had received Cabergoline (a dopamine receptor agonist on D2 receptors) for the past 4 months.
Examination
As above
Laboratory Investigations
| Date | Prolactin (mIU/L) |
| 02/2019 | 106 (Recovery of 80% following PEG precipitation) |
| 05/2019 | 135 |
| 06/2019 | 85 |
| 08/2019 | 1.3 (1.59 with a 1:10 dilution; 3.94 with a 1:50 dilution) |
Other Investigations
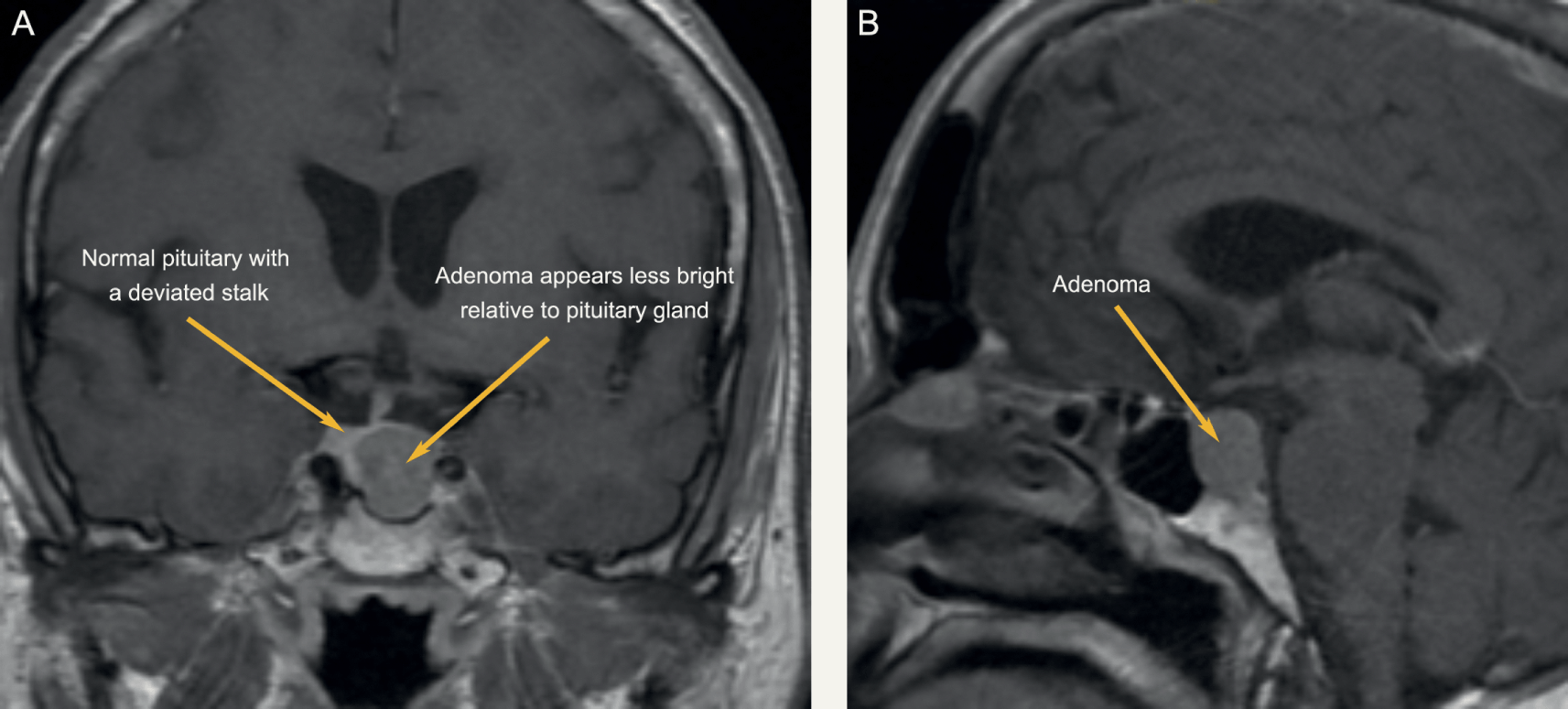
MRI Head was booked for the following week. Interestingly, even in prolactin secreting tumours, the correlation between tumour size and prolactin level is limited. MRI head remains a vital investigation.
Final Diagnosis
Take Home Message
During pregnancy the concentration of prolactin rises under the influence of elevated estrogen and progesterone production. The stimulating action of prolactin on the mammary gland leads post partum to lactation. Hyperprolactinemia (in men and women) is the main cause of fertility disorders. The determination of prolactin is utilized in the diagnosis of anovular cycles, hyperprolactinemic amenorrhea and galactorrhea, gynecomastia and azoo-spermia. Prolactin is also determined when breast cancer and pituitary tumors are suspected. As in this case, a pituitary tumour was suspected, hence the repeated prolactin results.
As was noted in another short case, our assay on the Roche platform does measure all forms of prolactin, and when a high result is obtained (above the gender-specific reference range) it is recommended to measure the recovery after PEG precipitation.

Dr. John Stanfliet (pathologist at Pathcare) repied to the above case with very valuable comments:
- We use Beckman Coulter DxI, an immunoassay that is not affected by macroprolactin (I’ve include an article that shows this).
- Even in prolactin secreting tumours, the correlation between tumour size and prolactin level is limited. MRI head remains a vital investigation.
- Some prolactin secreting tumours also secrete other pituitary hormones such as growth hormone.
- I would ascribe the reduction in PRL to the Carbegoline and wonder whether the dose has been increased.
- Dr. Pete Berman would often suggest a mixing study: find a sample with high PRL, mix it 50/50 with this sample, and measure it to see whether there is some interferant in this sample.
