A case of hyperuricemia in the ICU
| HOSP # | WARD | Surgical ICU | |
| CONSULTANT | Heleen Vreede / George van der Watt | DOB/AGE | 30 year Male |
Abnormal Result
The result upon the query being raised by the reviewer was a uric acid of 0.95 mmol/L (0.21-0.43 mmol/L). Three days prior to this result, the patient had a uric acid serum concentration of 0.38 mmol/L.
Presenting Complaint
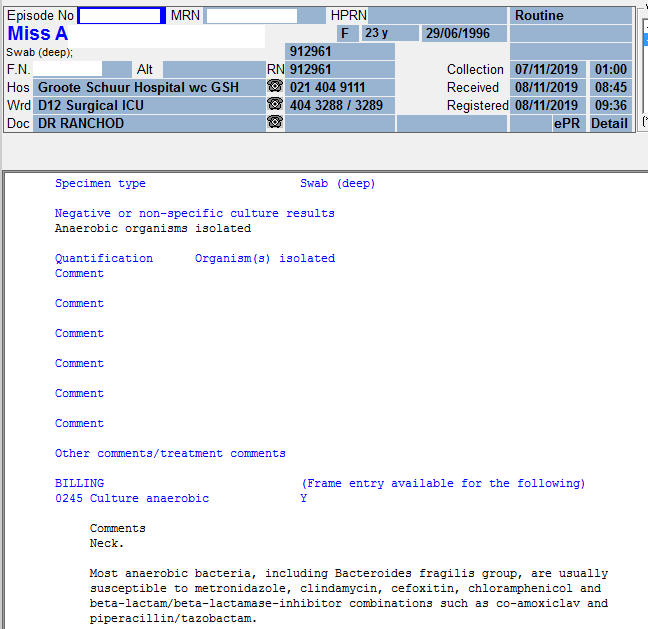
The patient presented to the hospital with a history of a swollen tonsil unilaterally. This worsened over few days to a severe infection (sepsis) as described below.
History
No significant history. Patient reported sober habits.
Examination
At initial presentation, the patient appeared to have a suppurative tonsillitis. The tonsillitis later developed into a retropharyngeal abscess and soon extended into the thorax, forming a pericardial abscess, which is what was found clinically at the time of admission to Groote Schuur Hospital.
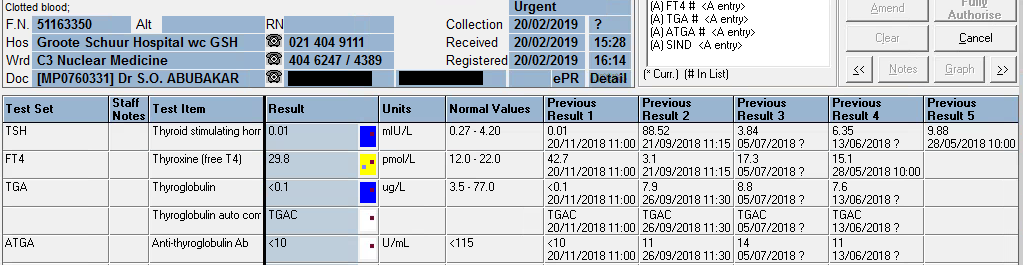
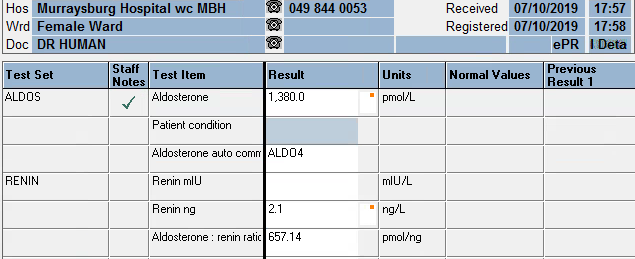
Laboratory Investigations
Date: newest to oldest (only chemistry results included)

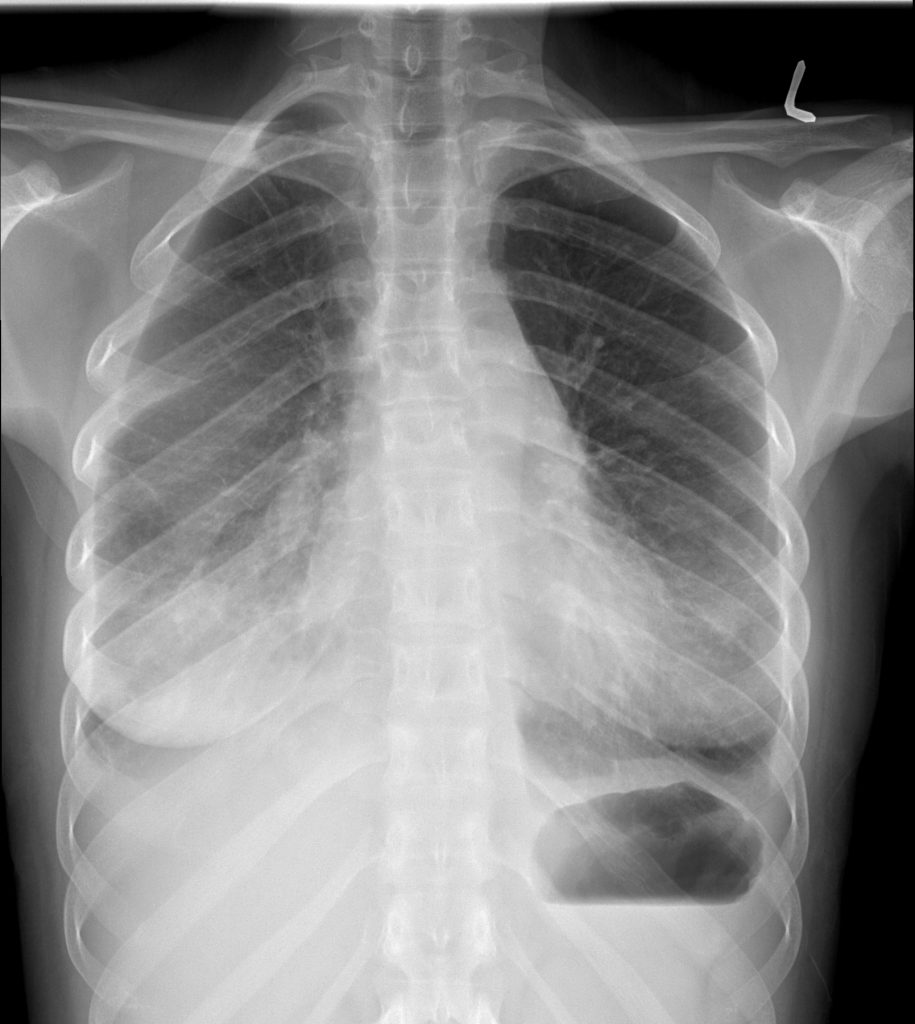
Other Investigations
CT scan: images to follow
Final Diagnosis
Retropharyngeal abscess progressing to a thoracic abscess and causing overt signs and symptons of heart failure.
Patient required a thoracotomy and pericardial drainage of the abscess.
Take Home Messages
- Do not take tonsillitis lightly. If not adequately managed, it may cause serious complications.
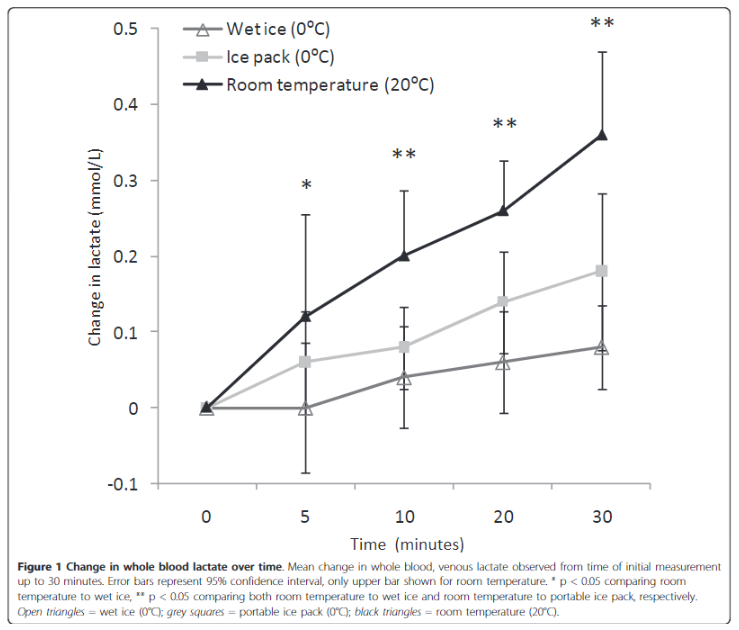
- Elevated Uric acid is a risk factor for acute kidney injury. This may be by means of acute gouty crystal deposition, but other crystal-independent roles has also been described.
- Uric acid concentration will rise significantly in severe infection, most likely due to the fast tempo of tissue or DNA turnover, both by bacteria and host tissue breakdown and repair. Uric acid is a product of the metabolic breakdown of purine nucleotides.
- Uric acid, being a heterocyclic compound, I thought could interfere in various assays, and I thought even in the Jaffe reaction for creatinine, but it doesn’t seem to be a common interferent when doing a quick literature search.
- Uric acid appears to be the major anti-oxidant in human serum constituting around 61% of total anti-oxidant activity, evidenced by Maxwell et al.:

- Relative contribution to total serum anti-oxidant activity in this study was: urate 65.1%, vitamin C 8.7%, vitamin E 10.6%, vitamin A 5.7%, thiols 7.8% (as in albumin) and bilirubin 1.9%.
- One immediately thinks that a patient with such a rapidly progressing infection has to be immunocompromised, the most common cause(s) in South Africa being HIV or diabetes mellitus. This patient however was HIV negative, according to HIV ELISA and did not have reported signs and symptoms of diabetes.